Abstract
Introduction: People with Hemophilia (PwH) have decreased bone mineral density (BMD) and increased risk of fracture. Children as well as adults have demonstrably lower BMD than age-matched control populations. Additionally, PwH have increased rates of bone resorption and decreased rates of bone mineralization. This study aims to characterize the impact of factor VIII (FVIII) replacement on biomarkers of bone metabolism in PwH as well as correlate those biomarkers with physical characteristics and Quality of Life.
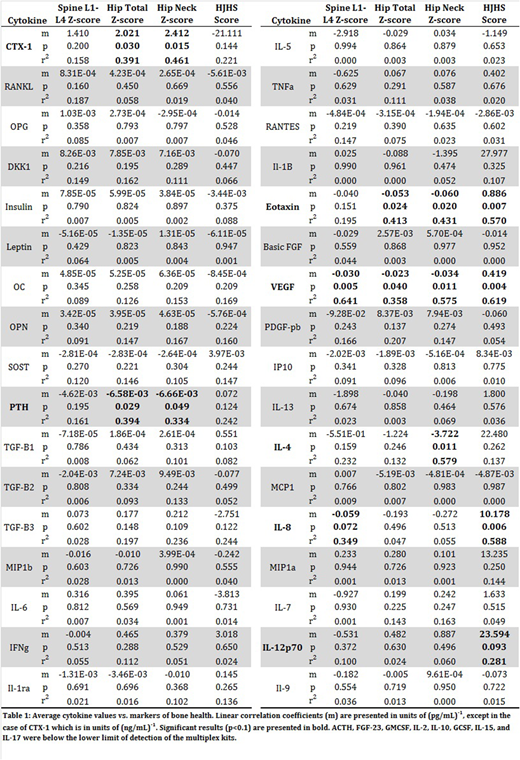
Methods: Twelve participants with severe FVIII-deficiency were screened and enrolled in the single site IRB-approved study. After a 72-hour washout, plasma samples were obtained at 8 time points over the course of five days following FVIII infusions on Day 1 (50 units/Kg) and Day 3 (20 units/Kg). All participants had a physical examination and completed quality of life, activity, pain and factor compliance questionnaires on Day 1. Visual Analog Scale (VAS) via the EQ-5D-5L was utilized to report participants' self-rated health. BMD was measured as Z-scores via Dual-Energy X-ray Absorptiometry (DEXA) Scanning. Joint assessment was performed using the Hemophilia Joint Health Score (HJHS). Plasma cytokine levels were measured using ELISA and magnetic bead multiplex kits. Samples were evaluated for 42 cytokines (Table 1).
Results: VAS score increased with Spine L1-L4 Z (SZ)-score (p=0.023, R2=0.42) and Hip Total Z (HTZ)-score (p=0.006, R2=0.54). VAS was lower in PwH with higher HJHS (p=0.006, R2=0.55). HJHS was higher in PwH with lower SZ-scores (p=0.004, R2=0.62). The average ratio of OPG to RANKL increased from 0.9 to 6.2 during the study period (p=0.006, R2=0.75). Plasma vascular endothelial growth factor (VEGF), an angiogenic cytokine that has been implicated in bone development and repair, and IL-8, a chemokine that stimulates osteolysis, inversely correlated with SZ-score. Carboxy-terminal collagen crosslinks (CTX-1), a breakdown product of bone, is elevated in samples from subjects with higher Hip Neck Z (HTZ)-scores. Eotaxin, an eosinophil chemoattractant, and VEGF levels were decreased in samples from subjects with lower HTZ-scores. CTX-1 levels were elevated in subjects with higher HNZ-scores. Parathyroid hormone (PTH), a hormone that stimulates osteolysis, eotaxin, VEGF, and IL-4, a potential osteoblast activity mediator, levels were lower in plasma samples from subjects with higher HNZ-scores. Average plasma eotaxin, VEGF, and IL-12p70, a T-cell stimulating factor, levels were positively correlated with HJHS score. Correlation coefficients, p-values and R2 values for average cytokine values and skeletal health measures are listed in Table 1.
Conclusions: PwH with decreased BMD report a lower level of self-rated health. This is evidenced by correlations between VAS, HJHS, and BMD. Plasma CTX-1 is elevated in PwH with higher BMD, suggesting that PwH with improved skeletal health experience higher rates of bone turnover as measured by osteoclast activity. The average OPG/RANKL ratio increased during the study period suggesting that FVIII infusion may have a direct effect on the RANKL-OPG pathway. PTH, eotaxin, and VEGF are inversely correlated with BMD and positively correlated with HJHS. Lower levels of these cytokines appear to be associated with poor skeletal health in PwH. Increased levels of PTH are associated with osteoporosis and VEGF has been implicated in bone development and repair. These data suggest an intricate association between skeletal health, factor administration, and cytokine levels. Continued analysis of these data is ongoing and additional findings will be discussed.
Lattimore:UniQure BV: Research Funding. Taylor:Bioverativ: Membership on an entity's Board of Directors or advisory committees; Shire: Research Funding; Alnylam: Research Funding; CSL: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal